Introduction
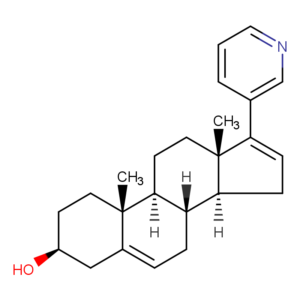
As a manufacturer of pharmaceutical intermediates and active ingredients, Abiraterone (CAS: 154229-19-3, C₂₄H₃₁NO, MW 349.52 g/mol) intermediates play an important role in the field of tumor treatment.
This blog takes a deep dive into its mechanism of action, side effects, and focuses on the intermediate stage – the basic chemistry that realizes its therapeutic potential.
Whether you are a researcher, formulator or procurement expert, understanding how Abiraterone works at the molecular level is key to optimizing the supply chain and ensuring the efficacy of the API.
Abiraterone’s Mechanism of Action: Blocking Hormone Fuel
Abiraterone targets prostate cancer by disrupting androgen synthesis. Unlike finished drug preparations, the intermediate form highlights its core function: inhibiting CYP17 enzymes.
These enzymes catalyze two key steps in steroid production – 17α-hydroxylation and C17,20-lyase reactions. By blocking CYP17, abiraterone can stop testosterone production and deprive hormone-sensitive prostate tumors of growth signals.
When we peel off the cold terms of scientific literature, we will find that the therapeutic magic of abiraterone begins with its unique “molecular dance”. In the battlefield where tumor cells proliferate wildly, it accurately locates the key hub of androgen synthesis – CYP17 enzyme.
This enzyme is like a power plant for tumor cells, constantly delivering “fuel” to maintain the growth of cancer cells. And the mechanism of action of abiraterone is just like an experienced bomb disposal expert, who instantly shuts down this power plant through irreversible binding.
Abiraterone Side Effects: Balancing Therapeutic Benefits with Patient Well-being
While abiraterone acetate has revolutionized the treatment landscape for metastatic castration-resistant prostate cancer (mCRPC), its clinical utility must be weighed against potential adverse effects. Understanding these side effects is critical for optimizing patient care and ensuring adherence to therapy.
The most frequently reported side effects of abiraterone often stem from its mechanism of action—inhibiting androgen synthesis while paradoxically increasing mineralocorticoid activity. Patients may experience fatigue, peripheral edema, and hypertension due to fluid retention and electrolyte imbalances.
Hypokalemia (low potassium) is particularly common, occurring in up to 25% of cases, and may exacerbate muscle weakness or cardiac arrhythmias. Regular monitoring of blood pressure, electrolytes, and renal function is essential during the initial weeks of treatment to mitigate these risks.
Hepatotoxicity represents another key concern, with elevated liver enzymes observed in approximately 10-15% of patients. While severe liver injury is rare, baseline and periodic liver function tests are advised, especially in those with pre-existing hepatic impairment. Clinicians should counsel patients to report symptoms like jaundice, dark urine, or abdominal pain promptly.
Less common but serious side effects include adrenal insufficiency, particularly in patients with prior ketoconazole use or underlying adrenal dysfunction. Signs such as nausea, vomiting, or hypotension warrant immediate evaluation. Additionally, abiraterone’s interaction with glucocorticoid therapy necessitates careful dose adjustments to avoid cortisol suppression.
Patient education plays a pivotal role in managing these challenges. Encouraging a low-sodium diet, potassium supplementation (under medical guidance), and moderate physical activity can alleviate fatigue and edema. Open communication about potential side effects empowers patients to seek timely intervention, improving quality of life without compromising oncologic outcomes.
The Takeaway
Mastering abiraterone therapy isn’t about eliminating side effects – it’s about anticipating them. Through smart monitoring and patient partnership, we can help men live with their treatment, not just through it. After all, beating cancer means preserving life’s quality as fiercely as we extend its quantity.